33 States Join Medicaid's Pay-Only-If-It-Works Model
Eighteen-year-old Serenity Cole spent Christmas with family instead of in the hospital, thanks to a groundbreaking gene therapy that could cure her sickle cell disease. The federal government is now making states pay for the $2-3 million treatment only if it actually works.
Last Christmas, Serenity Cole was stuck in a hospital bed battling sickle cell disease pain that had tormented her for years. This year, the 18-year-old from St. Louis was making crafts with family and hanging out with friends, living the normal teenage life that once seemed impossible.
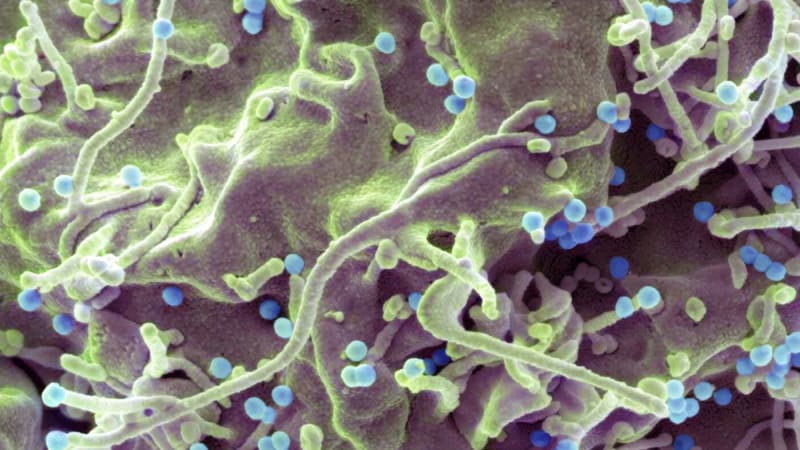
The difference? A gene therapy treatment that reprograms her body to produce healthy red blood cells instead of the damaged ones that caused her constant pain.
Serenity became one of the first Medicaid patients nationwide to receive treatment under a revolutionary payment model. The federal government negotiated a deal where drugmakers only get fully paid if their treatments deliver results.
It's a complete flip from how healthcare usually works. Typically, insurance companies pay the full price whether a drug helps patients or not.
The two approved gene therapies cost between $2.2 million and $3.1 million per patient, not counting hospital stays. For Medicaid programs that cover about half of the 100,000 Americans with sickle cell disease, mostly Black patients, those price tags are staggering.
Under the new agreements with manufacturers Vertex Pharmaceuticals and Bluebird Bio, states get discounts and rebates if the treatments fail. The federal government keeps the exact financial terms confidential, but 33 states, Washington D.C., and Puerto Rico have already signed on.

The timing matters enormously. Hundreds of cell and gene therapies are currently in clinical trials, with dozens expected to gain approval in coming years. Without a sustainable payment model, Medicaid programs could face impossible choices about covering breakthrough treatments.
Sickle cell disease already costs the healthcare system nearly $3 billion annually in emergency visits, hospitalizations, and other care. The condition shortens lifespans by more than two decades and causes strokes, organ damage, and debilitating daily pain.
For Serenity, the constant pain made planning anything feel impossible. School days were frequently interrupted. Social plans got canceled. Every single day hurt, even if some were more tolerable than others.
The gene therapies offer something families have desperately hoped for: a potential cure. But clinical trials included fewer than 100 patients and only tracked them for two years, leaving questions about long-term success.
The Ripple Effect
Maryland's Medicaid program plans to start accepting patients this month. Dr. Djinge Lindsay, the state's chief medical officer, explained their focus simply: whether services actually improve health.
If this model succeeds with sickle cell treatments, similar outcome-based agreements will likely follow for other expensive therapies, especially those treating rare diseases. The approach earned rare bipartisan support, continuing from the Biden administration into the current one.
Dr. Mehmet Oz, the current CMS administrator, called the model "a game changer" when announcing the 33-state participation. Health policy experts see it as a worthy experiment that could reshape how America pays for innovation.
For families like Serenity's, the policy details matter less than the results: a teenager who can finally plan a future without constant pain.
More Images


Based on reporting by Google News - New Treatment
This story was written by BrightWire based on verified news reports.
Spread the positivity! 🌟
Share this good news with someone who needs it