New Brain Tumor Surgery Standards Double Survival Time
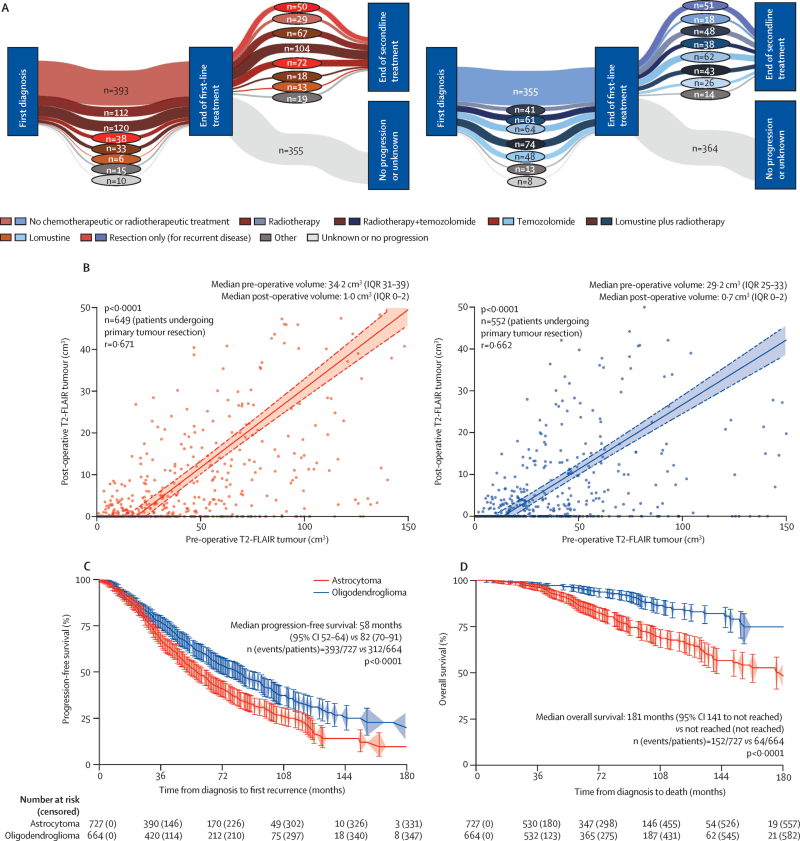
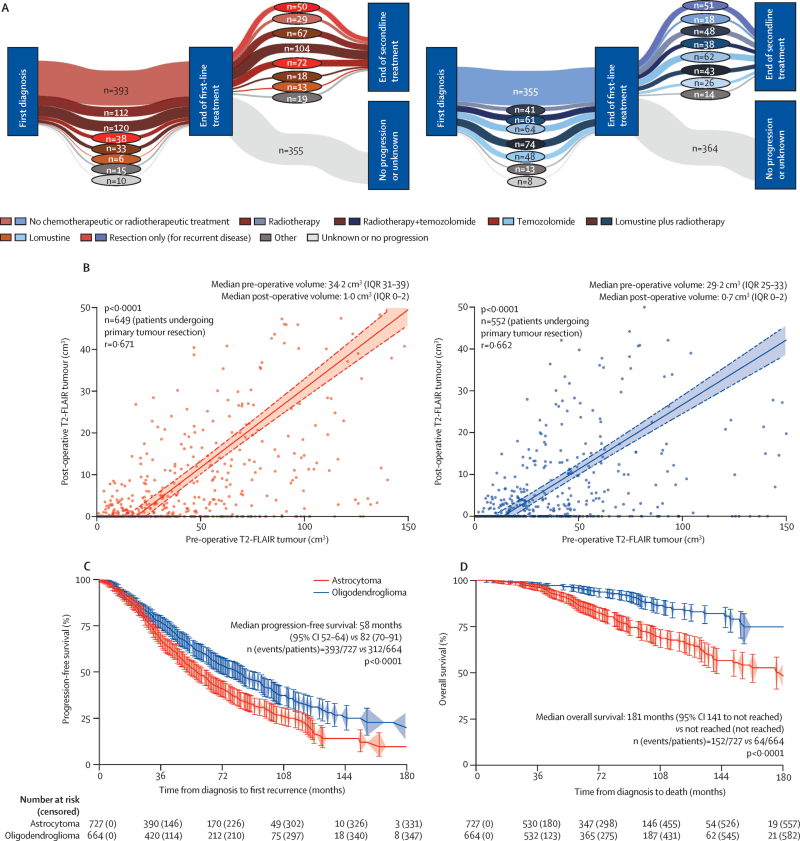
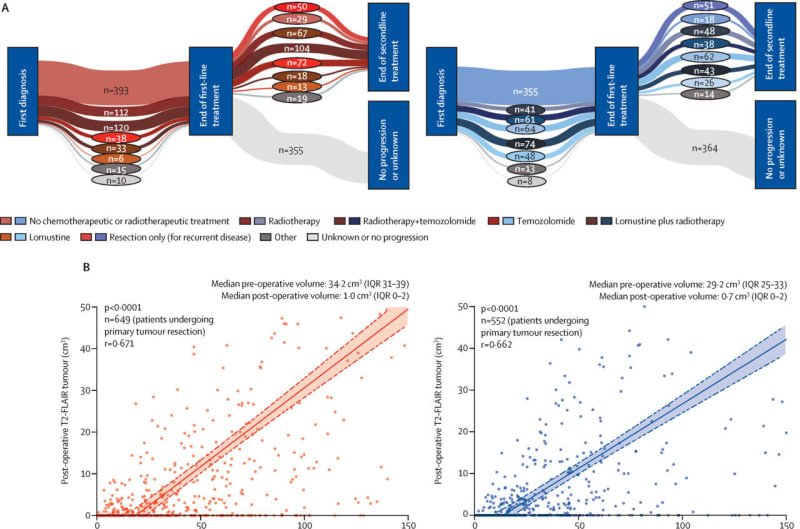
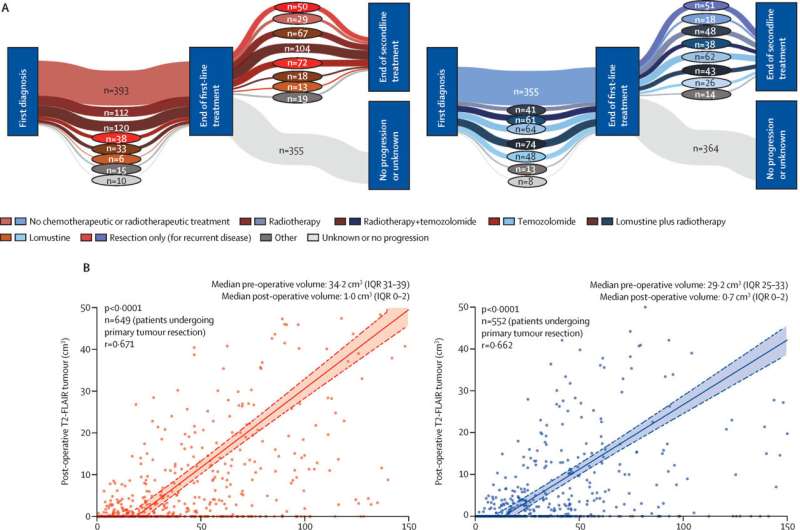
Surgeons now have a proven roadmap for removing brain tumors more safely and effectively, thanks to breakthrough research analyzing 1,391 patients across 16 medical centers. The new classification system shows that removing more tumor tissue dramatically extends survival, even for tumors once thought too risky to touch.
Brain surgeons have been walking a tightrope for decades, trying to remove deadly tumors without damaging the parts of the brain that make us who we are. Now, for the first time, they have a clear guide that shows exactly how much tissue to remove for the best chance at survival.
An international team of researchers studied nearly 1,400 patients with slow-growing but life-threatening brain tumors called IDH-mutant gliomas. They discovered something surprising: the less tumor left behind after surgery, the longer patients lived, and this held true even for tumor types previously treated with extreme caution.
"Until now, there was no common language available for describing surgical outcomes," explains Dr. Philipp Karschnia from Uniklinikum Erlangen, who helped lead the study. Different hospitals had wildly different approaches, ranging from removing just a tiny sample for diagnosis to taking out as much as possible.
The new RANO classification changes everything by measuring success based on how much tumor remains visible on MRI scans after surgery. This simple, objective standard replaces years of guesswork and conflicting treatment philosophies.
What shocked researchers most was that even powerful treatments like chemotherapy and radiation couldn't make up for leaving too much tumor behind. The initial surgery turned out to be far more important than anyone realized.
The research team, part of the Response Assessment in Neuro-Oncology working group, analyzed data from 16 specialized brain centers worldwide. Their findings were then confirmed by an independent group at the University of California, San Francisco, proving the results work across different hospitals and patient populations.
The Ripple Effect
This breakthrough gives surgeons the confidence to be more aggressive when it's safe to do so, potentially adding years to patients' lives. Families facing these terrifying diagnoses now have evidence-based hope instead of uncertainty.
The new system also paves the way for better clinical trials, since researchers can now compare results using the same measuring stick. Future treatments will be tested against a clear, universal standard.
Professor Oliver Schnell from Uniklinikum Erlangen calls it "a milestone that will make a significant impact on neuro-oncological research and care in the long term." After more than a decade of collaboration between experts worldwide, patients finally have what they desperately needed: clarity about the best path forward when facing one of medicine's toughest challenges.
More Images
Based on reporting by Medical Xpress
This story was written by BrightWire based on verified news reports.
Spread the positivity! 🌟
Share this good news with someone who needs it